Epidemiological Component

Objective
To determine the species of infection and key risk factors for infection, blood surveys and risk factor analysis based on demographics were conducted.
Methodology
Passive case detection (PCD) in health facilities was completed to analyse clinical malaria incidence during the study period. An analysis of historical data to understand how transmission levels had changed over time was undertaken.
Cross-sectional prevalence surveys were conducted in Thailand in the three study villages at four time points during 2016, as part of a concurrent study by Mahidol University. In Viet Nam, these surveys took place in August 2016.
Knowledge, attitudes and practices (KAP) surveys were undertaken at household level among the target villages in September 2016 in Thailand, and in August 2016 in Viet Nam.
Key findings: Thailand
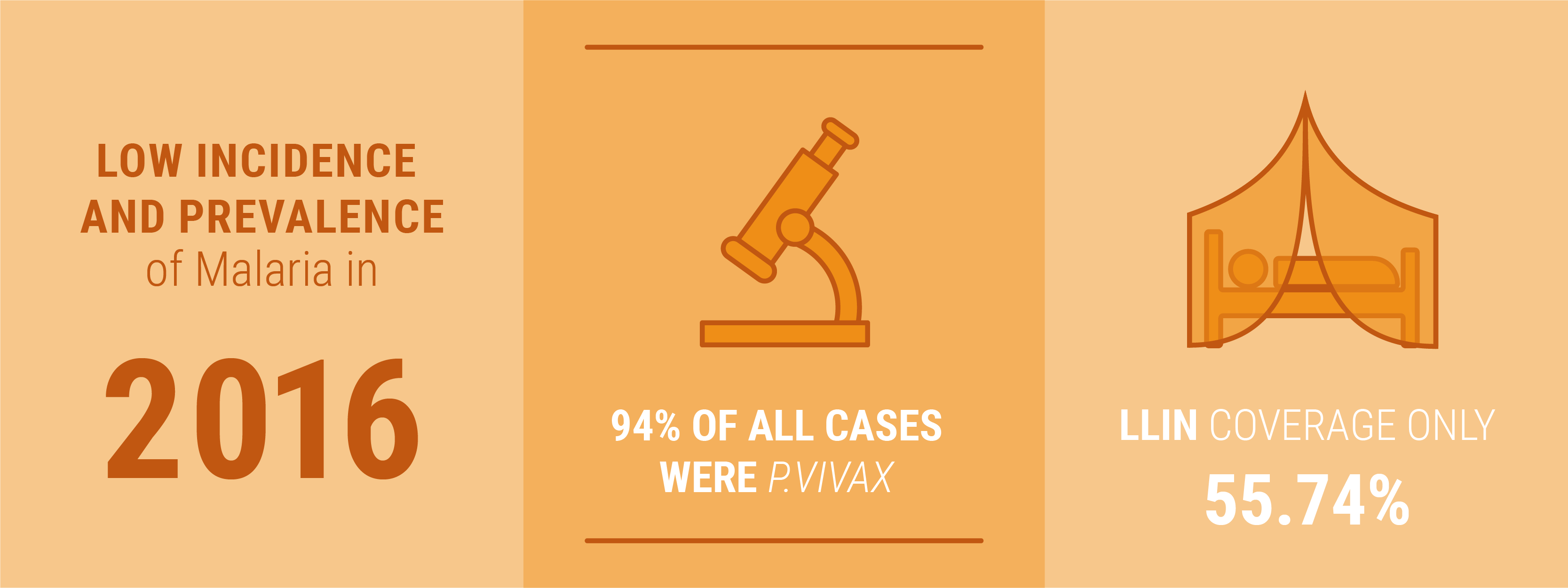
The incidence of malaria – or the total number of cases - was very low in 2016 compared to 2015.
Malaria prevalence – or the proportion of cases out of every 1000 people - was very low.
P. vivax was the dominant species of infection.
Locally transmitted malaria cases made up the majority of all cases.
Villages did not have universal LLIN coverage.
One third of adults staying overnight on the farm reported that they did not use a net the last time they stayed there.
Almost all of those who stayed overnight in the forest reported that they did not use a net.
Large variation in sleeping times meant that there was overlap with mosquito biting hours.
Key findings: Viet Nam
Malaria incidence – or total number of cases - was slightly higher in 2016 compared to 2015.
The prevalence of malaria – or the proportion of cases out of every 1000 people - was low.
P. falciparum was the dominant species of infection.
Universal LLIN coverage had not been achieved.
Usage of nets the previous night was very high, but the types of nets used were unknown.
Half of farm-goers either never or rarely used nets in the field or farm plot.
Most forest-goers did not regularly use nets in the forest.


